Prepatellar bursitis (Popeye knee/ carpenters’ knee)
What is this condition?
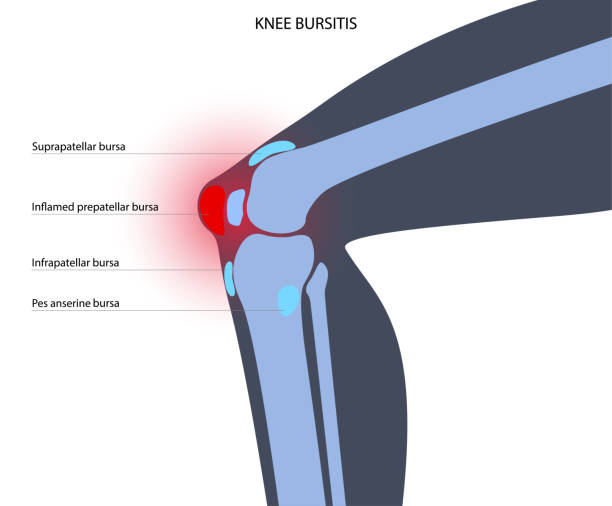
Prepatellar bursitis is the inflammation of the bursae directly overlying the patella in between the patella and the subcutaneous tissue. The bursae are fluid-filled sacs that act as a gliding surface for tissues in the body. Specifical the prepatellar bursae acts to protect the patella and quadriceps tendon from the friction that would be caused by flexion and extension-based movements. Due to its positioning, the prepatellar bursae have the second largest incidence of bursitis in the body, behind the olecranon bursae in the elbow (Rishor-Olney & Pozun, 2020)
What causes this condition?
Bursitis is commonly split into two major categories: non-septic bursitis (NSB) and Septic bursitis (SB). NSB is an inflammation of the synovial fluid-filled sac secondary to either acute trauma or overuse injuries in population groups that are commonly on their knee (Baumbach et al., 2014). The acute trauma triggers an inflammatory process that causes an overproduction of fluid within the bursae and subsequent swelling. Most susceptible athletes are wrestlers, volleyballers and basketballers, due to the nature of the sports and the surfaces they are played on. For an occupational population, gardeners, roofers, and carpenters have the highest’s incidence rate (Rishor-Olney & Pozun, 2020). Therefore, the layman’s term for prepatellar bursitis is the Carpenters knee or Popeyes knee due to its appearance.
Conversely, Septic Bursitis is caused by a bacterial infection of the bursae sac. This is most commonly cases by a skin lesion over the kneecap or a secondary spread from initial cellulitis. The occurrence of SB is not surprisingly 50% in immunocompromised patients (Huang & Yeh, 2011).
Common symptoms / signs
– Pain on palpation of the prepatellar bursae
– Popeye-like swelling over the patella
– Differential warmth over the kneecap
– Decrease ROM of the knee joint, limited by pain.
– If SB, pain associated with Fever and chills.
Common Differential diagnosis:
– Pseudogout
– Osteoarthritis
– Rheumatoid arthritis
– Gout
– Patella ligament rupture
– PFP
– Cruciate/collateral ligament injury
– Fractures
Risk factors of this condition?
– Occupation (NSB)
– Past-history of Bursitis
– Excessive knee trauma (NSB)
– Immunocompromised (SB)
Diagnostic process:
Detailed history for the patients needs to be taken including occupation, the onset of symptoms, pain patterns and effect on ADLs. A physical examination should also be conducted to narrow the differential diagnosis. Acute NSB present with pain on palpation whilst chronic NSB does not. If suspicion is raised surrounding possible infection, fevers, or chills, refer to GP for appropriate blood tests. Depending on the patient’s weight-bearing status and level of function, referral for an x-ray, MRI or CT may be required to rule out fractures or other ligamentous/soft tissue injuries.
How is it treated?
If SB is presented, medical management intervention should be undertaken to treat the underlying causes. For NSB, conservative management should be undertaken. For acute cases, being with therapies such as relative rest, ice, tub grip for compression, ADL modification and NSAIDs to reduce inflammation of the bursae. Education is also critical to preventing reaggravation, education will mostly consist of prevention strategies such as protective knee pads and precautions to avoid future knee trauma. Immobilization of the patient should last for about 1 week(Baumbach et al., 2014). For chronic conditions, conservative management should also be the first line of treatment. Once the swelling has subsided, an early exercise program is required to prevent the significant muscle loss that occurs during immobilization (Wall et al., 2015).
To start, isometric strength exercises such as a static knee extension and flexion should be considered to reduce the risk of reaggravation of the bursae. Hip and ankle exercises such as calf raises and hip flexion/extension/abduction should be considered to keep the surrounding musculature from atrophying, addition resistances with bands may be necessary depending on the patient’s pre-morbid strength. Additionally, low load AAROM exercise and Lower limb stretches should be introduced into the program early, preventing the stiffening of the knee joint. Progress these exercises over the coming weeks to add more load and dynamic balance, if reaggravation and subsequent inflammation appears, regress exercises with relative rest.
Surgical management may be required in cases where conservative and exercise-based management has failed to reduce pain and inflammation. Potential surgeries option included arthroscopic drainage of the bursae or a bursectomy in chronic cases. Return to exercise-based management should be undertaken post-surgery (Huang & Yeh, 2011).
References:
Baumbach, S. F., Lobo, C. M., Badyine, I., Mutschler, W., & Kanz, K. G. (2014). Prepatellar and olecranon bursitis: Literature review and development of a treatment algorithm. Archives of Orthopaedic and Trauma Surgery, 134(3), 359–370. https://doi.org/10.1007/s00402-013-1882-7
Huang, Y. C., & Yeh, W. L. (2011). Endoscopic treatment of prepatellar bursitis. International Orthopaedics, 35(3), 355–358. https://doi.org/10.1007/s00264-010-1033-5
Rishor-Olney, C. R., & Pozun, A. (2020). Prepatellar Bursitis Pathophysiology. 5–9. https://www.ncbi.nlm.nih.gov/books/NBK557508/
Wall, B. T., Morton, J. P., & van Loon, L. J. C. (2015). Strategies to maintain skeletal muscle mass in the injured athlete: Nutritional considerations and exercise mimetics. European Journal of Sport Science, 15(1), 53–62. https://doi.org/10.1080/17461391.2014.936326
Wilson, C. (2021). Prepatellar Bursitis Treatment. https://www.knee-pain-explained.com/prepatellar-bursitis.html
