Medial Collateral Ligament (MCL) / Lateral Collateral Ligament (LCL) Injuries:
What is this condition? What causes this condition?
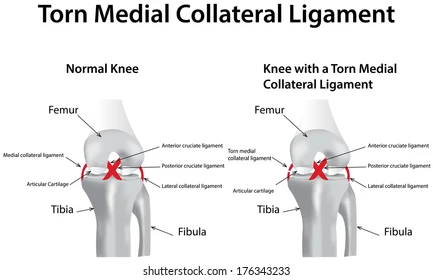
The MCL is a large ligament located on the medial aspect of the knee which functions to provide stability against valgus, internal and external torque loads (Hassebrock et al., 2020). An MCL injury can either be a stretch, partial or complete tear of the ligament and is commonly caused by a valgus stress to a partially flexed knee (Coleman, 2021). An MCL injury can be graded either I, II or III (Logerstedt et al., 2017):
- Grade I = <10% of torn collagen fibres, some tenderness but no instability, mild medial knee pain, possible swelling, and limping
- Grade II = tenderness but no instability, moderate medial knee pain, swelling, limping and instability
- Grade III = complete rupture resulting in instability, severe medial knee pain and swelling, knee gives way into valgus
The LCL is a cord-like band that acts as the primary varus stabiliser of the knee. It belongs to a group of complex structures located on the lateral aspect of the knee, often referred as the ‘posterolateral corner’ (Hassebrock et al., 2020). An LCL injury is most caused by a varus directed blow to the anteromedial aspect of the knee (Coleman, 2021). Non-contact hyperextension and varus stress applied to the knee are fewer common causes of an LCL injury (Coleman, 2021). An LCL injury can also be graded I, II or III (Logerstedt et al., 2017):
- Grade I = Mild tenderness and pain over LCL, usually no swelling, no instability, or mechanical symptoms present, <5mm laxity on varus test
- Grade II = Significant tenderness and pain on lateral and posterolateral aspect of knee, swelling in LCL area, 5-10mm laxity on varus test
- Grade III = Varied pain levels, tenderness on lateral aspect of knee, subjective instability, significant swelling, >10mm laxity on varus test
Most MCL and LCL injuries can be managed conservatively with bracing and rehabilitation, but surgical intervention is required for complete tears (Ng, Myint & Ali, 2020).
Common symptoms / signs
Common signs and symptoms experienced when a MCL injury is present include (Logerstedt et al., 2017):
- Pain and swelling on medial aspect of the knee
- Laxity at the medial knee when a valgus stress is applied
- Feeling like the knee is loose or wobbling
- Possible stiffness that may lock or catch with movement
- Positive valgus stress test at 0o or 30o of knee flexion
Common signs and symptoms experienced when a LCL injury is present include (Logerstedt et al., 2017):
- Lateral knee pain
- Localised swelling over LCL
- Laxity at lateral knee when a varus stress is applied
- Possible varus instability with ambulation
- Positive varus stress test at 0o or 30o of knee flexion
Risk factors of this condition?
Risk factors of MCL or LCL injury mentioned by Kuikka, Pihlajamäki & Mattila (2013) include:
- Previous torn MCL/LCL
- Female sex
- High BMI
- Weak quadricep muscles
- Participation in certain sports such as soccer, football, hockey and basketball
- Contact and non-contact sports that involve tackling, cutting, pivoting or jumping
How is it treated?
Early rehabilitation strategies after MCL or LCL injury recommended by Logerstedt et al. (2017) include immediate mobilisation, cryotherapy, early weight-bearing, continuous passive motion, quadricep activation exercises and neuromuscular electrical stimulation. It is also advised to avoid applying significant stress to healing structures over 3-4 weeks after the injury to ensure the ligaments are provided sufficient time for recovery.
Late rehabilitation strategies discussed by Logerstedt et al. (2017) are summarised below:
|
Therapeutic Exercises |
· Range of motion, strength, flexibility and proprioception training in lower limb musculature · Closed chain strength work · Progression of strength exercises of quadriceps, glutes, gastrocnemius, and hamstrings · Plyometric exercises (with focus to reduce excessive valgus or varus) · Exercises to address the knee but also joints above and below (ankle, foot, hip, trunk) |
|
Neuromuscular Re-Education |
· Optimal neuromuscular training progression · Full weight-bearing and gait re-education |
|
Supervised Rehabilitation |
· High level strengthening and loading of the whole kinetic chain · Aerobic conditioning · Sport specific training |
|
Education Strategies |
· Indications for surgical intervention · Activity modification · Return-to-sport readiness and associated risks |
Surgical intervention is required for complete rupture of MCL or LCL (Ng, Myint & Ali, 2020).
Other causes?
MCL and LCL injuries can also be caused from agility-based activities where direction is rapidly changed and pivoting onto the one foot. This poses an intrinsic valgus/varus force onto the knee and can cause the ligament to sprain, partially or completely tear. Landing awkwardly from a jump can also cause a MCL or LCL injury to occur. Lastly, MCL or LCL injuries can also result from an ACL injury or direct blow to the knee where multiple ligaments can be damaged.
(Hassebrock et al., 2020)
References:
Coleman. (2021). Common Pediatric Knee Injuries: Best Practices in Evaluation and Management. Springer International Publishing AG.
Hassebrock, J. D., Gulbrandsen, M. T., Asprey, W. L., Makovicka, J. L., & Chhabra, A. (2020). Knee ligament anatomy and biomechanics. Sports medicine and arthroscopy review, 28(3), 80-86.
Kuikka, Pihlajamäki, H. K., & Mattila, V. M. (2013). Knee injuries related to sports in young adult males during military service – Incidence and risk factors. Scandinavian Journal of Medicine & Science in Sports, 23(3), 281–287. https://doi.org/10.1111/j.1600-0838.2011.01397.x
Logerstedt, D. S., Scalzitti, D., Risberg, M. A., Engebretsen, L., Webster, K. E., Feller, J., … & Zachazewski, J. (2017). Knee Stability and Movement Coordination Impairments: Knee Ligament Sprain Revision 2017: Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability and Health from the Orthopaedic Section of the American Physical Therapy Association. Journal of Orthopaedic & Sports Physical Therapy, 47(11), A1-A47.
Ng, J. W. G., Myint, Y., & Ali, F. M. (2020). Management of multiligament knee injuries. EFORT open reviews, 5(3), 145-155.
